Let’s get it clear: Pressure, Shear, and Friction
What’s the difference, how do they relate, and why should each be managed in their own right?
There has been an awareness for a long time that pressures in the wrong places can lead to damage to skin tissues, damage generally presenting as pressure ulcers.
With pressure, other damaging influences come into play, such as microclimate, friction, and shear.
In this article we look at what we mean by pressure, friction, and shear, and assess the respective influences each of these have on our skin tissues. Along the way, we hope to dispel some of the widely-held misconceptions which still exist.
The influence of pressure on the health of our skin has been acknowledged for some time: as a result, what used to be called bed sores or decubitus ulcers became renamed pressure ulcers in Europe and then pressure injuries in much of the rest of the world. However, in recent years, there has developed a greater awareness of the importance of other external factors, rather than pressure on its own, on the health of our skin tissues – and this has led to an increased reference to the more general term of tissue integrity in order that all the blame does not lie with pressure alone.
The other external factors that affect tissue integrity include microclimate (heat and moisture), shear forces, and friction. These factors do not have an impact without pressure bringing them into play, but it is these other external factors which currently are thought to be more influential in affecting the health of the outer layers of the skin, and giving rise Grade 1 and 2 ‘pressure ulcers’.
Thus, we know that ‘pressure’, ‘friction’, and ‘shear’ are important, but frequently these terms are misused, and for this reason, an ISO standard (ISO 16840-1) in the wheelchair seating series is being developed, to provide definitions for these terms, and discuss the implications of each element on skin health. This article presents some of the material from this draft standard and suggestions of the different effects that each element can have on the skin.
Pressure
The pressures that we experience on our skin come from the force of gravity pulling our body mass towards the ground, and the equal and opposite reaction from the surface that we are standing, sitting or lying on. The amount of pressure we experience depends on the area over which the force is spread.
If you push against the top of a drawing pin with a certain force, that force is spread over a wide area and is acceptable, whereas if you apply the same force over the point of the drawing pin, your force is over a very small area, and you get a painful hole in your finger! In seating and bedding, we are trying to spread the forces of gravity over as wide an area as possible to minimise the pressure – a domain in which we use pressure mapping, to see where the forces are going.

Pressure can compress various materials, such as our skin tissues, or the materials we are sitting on. For the amount that something is stretched or deformed, the term strain is used.
For the compression that occurs as a result of pressure, this is called axial strain (Fig 1), in that the deformation occurs along the axis of the force.
Friction
Friction is the force that ‘opposes the relative lateral movement of two surfaces in contact’, and from a seating point of view can be static (between non-moving surfaces) or dynamic friction. Static friction is what is stopping us from sliding out of our seats, and is generally a ‘good thing’.
On the other hand, when the forces resisting this lateral movement are overcome, and the surfaces start sliding over each other, the result is dynamic friction, which can damage the surface of the skin, such damage is sometimes referred to as friction ‘burns’ (for example when people’s feet are dragged across sheets as they are brought to the edge of a bed, to help them get out of bed, or for turning purposes).
Dynamic friction is generally a ‘bad thing’ where kinetic energy is being converted into thermal energy. Friction arises from a combination of ‘inter-surface adhesion’, ‘surface roughness’, and ‘surface deformation’, so what a cushion or bed cover is made of will have a direct effect on the skin.
Shear
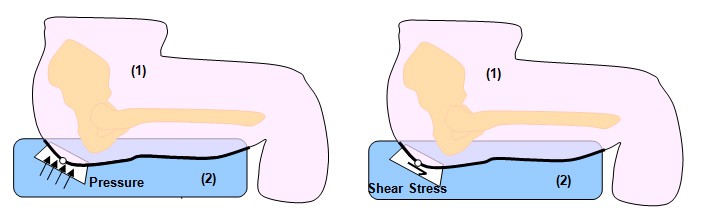
Shear is the sideways force that takes place at right angles to pressure (Fig. 2). Static friction, where skin and support surfaces meet, ‘grabs’ the respective surfaces and distorts the deeper materials sideways: this kind of distortion is called shear strain (Fig. 3).
What’s happening to, and in the skin?
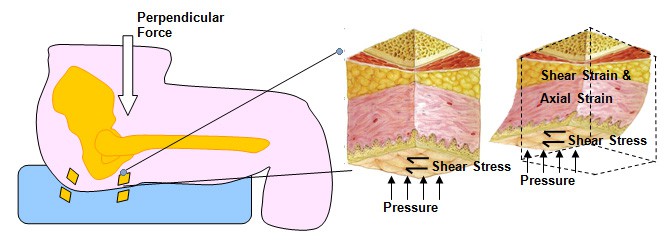
Figure 4 illustrates the deformities, or strains, that the skin tissues experience from the pressure and shear forces illustrated in Figure 2. There is a combination of the compressive forces of pressure creating axial strain, and the sideways effects of shear stress creating shear strain.
The axial strain from pressure on skin tissues can slow down the rate of flow in blood vessels and capillaries, and over days this can lead to cell death. Shear strain distorts the cells and cell walls, and result in cell content leakage, and imbalance of the cell contents, which in turn can lead to cell death even more rapidly, i.e. in less than a day.
Thus, the attendant effects of shear strain, alongside the pressures introduced by the effects of gravity creating areas of pressure on the body, have a faster and more damaging effect on the tissues themselves, than from pressure alone. Ideally, if the materials that a person is sitting or lying on can absorb or redistribute the axial and shear strains, they should reduce the strains that the skin has to accommodate.
Use of a selected mix of cover materials and deeper bed/cushion materials to redirect the forces to thicker skin areas (e.g. away from the pelvis to the thighs) where the forces can be spread over a larger area will be beneficial.
In conclusion
Being aware of the potentially damaging effects that pressure, friction, and shear each in their own and in related ways can have on the skin, and the effects that different support surfaces can have in ameliorating these effects, should lead the prescriber to more appropriate selection of seating and bed materials to meet an individual’s needs.
Further items can be found at www.beshealthcare.net. If you are interested in receiving further information on the topic, please contact barend@beshealthcare.net.
Dr Barend ter Haar has been involved in seating and mobility for over 30 years, including lecturing internationally and developing international seating standards.
Click to read more from the ‘Let’s get it clear’ series from Dr Barend ter Haar