Let’s get it clear: How can we get one size to fit all in seating?
Seating in long-term care facilities is seldom designed for the individual using it – often, all the chairs have been bought as a package and look smart when lined up and unoccupied.
In individual people’s homes, a person may have their favourite chair, but that chair may not be adequate for current needs. What can be done to customise this seating for better outcomes, but with the cooperation of the individuals and their carers?
The majority of wheelchair seating in long-term facilities has been reported to be inappropriate nearly 60 per cent of the time. Similar observations have been made around general seating in the same institutions. Common implications are discomfort, poor positioning and mobility, and skin integrity issues. Individuals in their own homes often have their ‘favourite’ chairs and are unwilling to change them for something their healthcare adviser might prescribe as being more appropriate.
So what can we do to ‘help the individuals help themselves’? In this article, we will address what needs to be done here, but also address the common problems and what we might be able to do around the existing seating provision that might lead to better outcomes.
What are the common problems?
Having a chair that has been purchased on the basis that ‘the one size will fit all’ usually means that ‘the one size fits no-one’! What are the problems that this presents?
- If the chair will accommodate the body mass of the largest plus-sized individual, then the odds are that the seat is too wide for the average person – who will then twist to try to get some lateral support on at least one side.
- If the chair will accommodate taller people, then the depth of the seat will be too large for the average person – who will slouch into a kyphotic position to try to get some support from the chair’s back.
- If the chair will accommodate taller people, then the cushion will be too high off the ground for the average person, leaving the average person’s feet off the ground – the pressure on the underside of the thigh can affect their venous return, leading to swelling of the feet. In addition, the unstable feeling of ‘legs dangling’ can be very distressing for the person, particularly if they have any proprioception deficits.
- To accommodate the circumstances in 3, a footstool is often provided. However, this extension of the legs for the feet to reach the stool, pulls on shortened hamstrings, which in turn pull forward on the individual’s pelvis, which, in turn, again leads to a kyphotic posture.
- If the height of the cushion is too low, on the other hand, then there will not be even distribution of the body’s
mass along the thighs, and the result is more pressure under the boney parts of the pelvis, potentially leading to tissue damage under the pelvis. In addition, this lower position makes it more difficult for the infirm to leave their seats. - The upholstery is often ‘incontinence-proof’ for easy cleaning. However, this usually means that the surface is smooth, and the individual then has problems that arise from sliding and struggling to maintain their position. Many durable upholstery coverings are quite rigid which prevents any level of immersion which reduces pressure redistribution, and also leaves the individual ‘perched’ on the surface. The impervious surface is often not breathable and thus leads to moisture and heat build-up next to the skin.
How can we address these problems?
First, the client needs to be part of the process. If they are not comfortable with the solution, the solution will not be used – this applies to both the seated individuals and to their carers. Below we will look at potential means to manage the problems listed above.
-
Fig. 1 A Jonvac back support The chair’s seating area is too large for the individual (1 and 2 above). Often, loose cushions or pillows are placed around the individual. However these move around, fall to the floor, and generally get in the way. More beneficial are the adjustable vacuum-formed solutions, where a bag, filled with polystyrene microbeads, is formed around the individual into the required comfortable position, and then the air sucked out of the bag to leave the beads in a fixed position (Fig. 1).
To adjust to different clients or different chairs, the air is let in again, the beads readjusted, and the air sucked out again. This can all be done with feedback from the seated individual as to whether they are comfortable, can move to carry out activities from the chair, etc. This customisation of the individual’s seating also allows the creation of a block at the top of the pelvis (at the PSISs) to help control the degree of posterior pelvic tilt and attendant kyphotic curvature of the spine.
As a note: a) Please make sure that the ‘bag’ has a suitable cover, not only for comfort and improved appearance for acceptance, but to allow the skin to breathe.
b) Using a pressure mapping system can help to assess the best balance between positioning and pressure distribution. In addition, the visual demonstration on screen of the benefits for the individual can really help improve acceptance of change. -
Fig. 2. An adjustable chair raiser The chair seat is too high off the ground (3 and 4). A foot step that takes the feet off the ground, but still allows the feet to come back under the edge of the chair, will fill the gap, but not have the foot position forward, thereby pulling on the hamstrings and pulling the individual into a kyphotic position. Foot stools have their place to help with reducing swelling of the feet, but then the chair back support will need to have a recline function.
- The chair seat is too low (5). A chair raiser may be the best option – an example is shown in Figure 2. These are not always the most attractive of solutions, but they are practical. Also, these can be easily stored away when not needed.
- The chair cover is too firm, slippery, or unbreathable (6). As discussed in an earlier article in this series, the body benefits when the interface with a seating surface is via natural
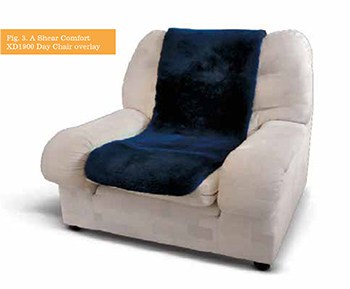
Fig. 3. A Shear Comfort
XD1900 Day Chair overlaymaterials. Medical sheepskins and pure wool-based overlays (provided they have sufficient wool density) provide a comfortable surface to sit on, with reduced shear forces on the skin and better temperature and water vapour control. An example is the XD1900 Day Chair overlay shown in Figure 3.
Patient concordance
As mentioned above, the solutions you offer, which allow the individual still to use their favourite chair, or with which they feel comfortable, are more likely to succeed than other ‘imposed’ solutions. Explaining in simple terms the downsides around what the person has been doing while discussing the benefits of alternatives will help in achieving concordance with your aims.
For some clients, using the images from a pressure mapping system helps show them in pictorial form what is going on around them and under them – however, it’s not just the clients who need to see these and hear the explanations, it’s also their carers.
References
- Canada S. Participation and Activity Limitation survey 2006. Ottawa: 2008
- Giesbrecht EM, Mortenson, WB, Miller W. Prevalence and facility level correlates of need for wheelchair seating assessment among long term care residents. Gerontology. 2012; 58:378-384
- Mortenson WB, Miller WC. The wheelchair procurement process: perspectives of clients and prescribers. Can J Occ Ther. 2008; 75:167–75.
- Bourbonniere MC, Fawcett, LM, Miller WC, Garden J, and Mortenson WB. Prevalence and predictors of need for seating intervention and mobility for persons in long-term care. Can J Aging. 2007; 26:195–204.
- Naturally – It’s material what one uses for pressure and skin care. THIIS 2020 September
40-43
Further items can be found at www.beshealthcare.net. If you are interested in receiving further information on the topic, please contact barend@beshealthcare.net.
Dr Barend ter Haar has been involved in seating and mobility for over 30 years, including lecturing internationally and developing international seating standards.
Click to read more from the ‘Let’s get it clear’ series from Dr Barend ter Haar
https://thiis.co.uk/lets-get-it-clear-how-can-we-get-one-size-to-fit-all-in-seating/https://thiis.co.uk/wp-content/uploads/2021/10/shear-comfort.jpghttps://thiis.co.uk/wp-content/uploads/2021/10/shear-comfort-150x150.jpgAnalysis & InsightsLet's Get It ClearNewsroomBES Healthcare,bespoke seating,Dr Barend ter Haar,Let's get it clear,seating sizing,Specialist seatingSeating in long-term care facilities is seldom designed for the individual using it – often, all the chairs have been bought as a package and look smart when lined up and unoccupied. In individual people’s homes, a person may have their favourite chair, but that chair may not be adequate...Sarah SarsbySarah Sarsbysarah@thiis.co.ukEditorTHIIS Magazine